Oxycodone, also available as OxyContin, is an opioid medication (sometimes called narcotics). It helps treat moderate to severe pain. The extended-release design of Oxycodone is for around-the-clock treatment of pain, and one should not use it on an as-needed basis for pain.
Chemical name: 4,5α-epoxy-14-hydroxy-3-methoxy-17-methylmorphinan-6-one hydrochloride.
CAS No.: 124-90-3.
Molecular formula (anhydrous form): C18H21NO4.HCl.
Molecular weight (anhydrous form): 351.83.
Molecular formula (monohydrate form): C18H21NO4.HCl.H20.
Molecular weight (monohydrate form): 369.84.
Oxycodone hydrochloride is a white, crystalline, odourless powder readily soluble in water, sparingly soluble in ethanol and nearly insoluble in ether.
Oxycodone HCl (OxyContin NEO) tablets are modified release tablets designed to provide delivery of oxycodone over 12 hours.
Oxycodone HCl (OxyContin NEO) 10 mg, 20 mg and 40 mg tablets have been reformulated, and comprise a matrix formulation with a hydrogelling property (i.e. particles or whole tablets become highly viscous (gel-like) in water), intended to be crush-deterrent and to reduce the rapid release of oxycodone upon accidental or intentional misuse. The tablets have been heat-treated to increase the mechanical strength of the tablet.
The physical properties of the reformulated Oxycodone HCl (OxyContin NEO) tablets were examined following an extensive battery of physical manipulations. Beyond demonstrating that the reformulated Oxycodone HCl (OxyContin NEO) tablets are harder to crush than another controlled release oxycodone formulation, testing over the range of the reformulated Oxycodone HCl (OxyContin NEO) tablets fragment sizes showed that some of the controlled release properties were still retained. Hydrogelling properties continued to be demonstrated.
Excipients/Inactive Ingredients: The inactive ingredients in the reformulated Oxycodone HCl (OxyContin NEO) 10 to 40 mg tablets are: polyethylene oxide, butylated hydroxytoluene (BHT) and magnesium stearate.
Film coating also contain: Opadry Y-5-18024-A White (US version) (ARPING No. 3548) (10 mg), Opadry YS-1-14518-A Pink (ARPING No. 3547) (20 mg) and Opadry Yellow YS-1-12525-A (ARPING No. 3550) (40 mg).
Opioids may influence the hypothalamic-pituitary-adrenal or -gonadal axes. Some changes that can be seen include an increase in serum prolactin and decreases in plasma cortisol and testosterone. Clinical symptoms may manifest from these hormonal changes.
Clinical trials: A double-blind, placebo-controlled, fixed-dose, parallel group, two-week study was conducted in 133 patients with persistent, moderate to severe pain, who were judged as having inadequate pain control with their current therapy. In this study, Oxycodone HCl (OxyContin NEO) 20 mg tablets, but not 10 mg tablets, was statistically significant in pain reduction compared with placebo.
Pharmacokinetics: Absorption: Compared with morphine, which has an absolute bioavailability of approximately 30%, oxycodone has a high absolute bioavailability of up to 87% following oral administration.
The mean apparent half-life of Oxycodone HCl (OxyContin NEO) tablets is 6.5 hours and steady-state is achieved in about one day.
Release of oxycodone from Oxycodone HCl (OxyContin NEO) tablets is independent of pH under physiological conditions. Oxycodone HCl (OxyContin NEO) tablets have an oral bioavailability comparable with immediate release oral oxycodone, but achieve maximal plasma concentrations at about three hours compared with 1-1.5 hours for immediate release oral oxycodone. Peak and trough concentrations of oxycodone from Oxycodone HCl (OxyContin NEO) tablets 10 mg administered 12-hourly are similar to those achieved from immediate release oxycodone 5 mg administered 6-hourly.
Dose proportionality has been established for the 10 mg, 15 mg, 20 mg, 30 mg, 40 mg, 60 mg and 80 mg tablet strengths for both peak plasma concentrations (Cmax) and extent of absorption (AUC).
Recent fasted and fed studies for Oxycodone HCl (OxyContin NEO) 10, 40 and 80 mg tablets indicate that food has no significant effect on the extent of absorption of oxycodone from Oxycodone HCl (OxyContin NEO) tablets.
Distribution: Following absorption, oxycodone is distributed throughout the entire body. Oxycodone has been found in breast milk (see Use in lactation under PRECAUTIONS & USE IN PREGNANCY & LACTATION).
Metabolism and Elimination: Oxycodone has an elimination half-life of approximately three hours and is metabolised in the liver to form noroxycodone, oxymorphone, noroxymorphone, 6 α and β oxycodol and conjugated glucuronides. CYP3A4 and CYP2D6 are involved in the formation of noroxycodone and oxymorphone, respectively (see INTERACTIONS). The contribution of these metabolites to the analgesic effect is insignificant.
Administration: Oxycodone HCl (OxyContin NEO) tablets are to be swallowed whole, and are not to be cut, broken, chewed, crushed or dissolved. The tablets have been hardened to reduce the risk of being accidently or intentionally broken, chewed or crushed. Taking cut, broken, chewed, crushed or dissolved Oxycodone HCl (OxyContin NEO) tablets could lead to the rapid release and absorption of a potentially fatal dose of oxycodone.
To avoid difficulty swallowing, Oxycodone HCl (OxyContin NEO) tablets should not be pre-soaked, licked or otherwise wetted prior to placing in the mouth and should be taken one tablet at a time with enough water to ensure complete swallowing immediately after placing it in the mouth.
There are no data on rectal administration of Oxycodone HCl (OxyContin NEO) tablets, therefore rectal administration of Oxycodone HCl (OxyContin NEO) tablets is not recommended.
Do not administer Oxycodone HCl (OxyContin NEO) tablets via nasogastric, gastric or other feeding tubes as it may cause obstruction of feeding tubes.
Alcoholic beverages should be avoided by patients while being treated with Oxycodone HCl (OxyContin NEO) tablets.
Adults, elderly and children over 12 years: Prior to initiation and titration of doses, refer to the PRECAUTIONS section for information on special risk groups such as females and the elderly. Oxycodone HCl (OxyContin NEO) tablets should be taken at 12- hourly intervals. Appropriate pain management principles of careful assessment and ongoing monitoring should be followed at regular intervals, including reassessing the need for continued opioid therapy. The dosage is dependent on the severity of the pain, and the patient’s previous history of analgesic requirements.
The usual starting dose for opioid-naïve patients or patients presenting with moderate to severe pain uncontrolled by weaker opioids (especially if they are receiving concurrent sedatives, muscle relaxants or other CNS medicines) is 10 mg 12-hourly.
The dose should then be carefully titrated with longitudinal patient monitoring, assessing whether the pain is opioid responsive and providing the patient significant pain relief.
Increasing severity of pain may require an increased dosage of Oxycodone HCl (OxyContin NEO) tablets to achieve a stable dose that provides acceptable pain relief. The correct dosage for any individual patient is that which controls the pain and is well tolerated, for a full 12 hours. If higher doses are necessary, increases should be made, where possible, in 25%-50% increments.
Patients who experience breakthrough pain may require dosage adjustment or rescue medication. The need for rescue medication more than twice a day indicates that the patient should be reassessed and, only if appropriate, the dosage of Oxycodone HCl (OxyContin NEO) tablets should be increased. There are no well-controlled clinical studies evaluating the safety and efficacy with dosing more frequently than every 12 hours.
Patients receiving oral morphine before Oxycodone HCl (OxyContin NEO) tablet therapy should have their daily dose based on the following ratio: 10 mg of oral oxycodone is equivalent to 20 mg of oral morphine. It is emphasized that this is a guide to the dose of Oxycodone HCl (OxyContin NEO) tablets required only. Inter-patient variability requires that each patient is carefully titrated to the appropriate dose.
Controlled pharmacokinetic studies in elderly patients (aged over 65 years) have shown that compared with younger adults the clearance of oxycodone is only slightly reduced. No untoward adverse drug reactions were seen based on age, therefore adult doses and dosage intervals are appropriate.
Children under 12 years: Oxycodone HCl (OxyContin NEO) tablets are not recommended for children under 12 years of age.
Patients with renal or hepatic impairment: The dose initiation should follow a conservative approach in these patients. The recommended adult starting dose should be reduced by ⅓ to ½, and each patient should be titrated to adequate pain control according to their clinical situation (see Special Risk Groups under PRECAUTIONS).
Patients transferring from other opioid formulations: Patients receiving other oral oxycodone formulations may be transferred to Oxycodone HCl (OxyContin NEO) tablets at the same total daily dosage, equally divided into two 12-hourly Oxycodone HCl (OxyContin NEO) tablet doses. For patients who are receiving an alternative opioid, the “oral oxycodone equivalent” of the analgesic presently being used should be determined. Having determined the total daily dosage of the present analgesic, the following equivalence table can be used to calculate the approximate daily oral oxycodone dosage that should provide equivalent analgesia. The total daily oral oxycodone dosage should then be equally divided into two 12-hourly Oxycodone HCl (OxyContin NEO) tablet doses. (See Table 1).
 Click on icon to see table/diagram/image
Click on icon to see table/diagram/imageTreatment: Primary attention should be given to immediate supportive therapy with the establishment of adequate respiratory exchange through the provision of a patent airway and institution of assisted or controlled ventilation. Adequate body temperature and fluid balance should be maintained. Oxygen, intravenous fluids, vasopressors and other supportive measures should be used as indicated, to manage the circulatory shock accompanying an overdose. Cardiac arrest or arrhythmias may require cardiac massage or defibrillation.
Activated charcoal may reduce absorption of the drug if given within one to two hours after ingestion. Administration of activated charcoal should be restricted to patients who are fully conscious with an intact gag reflex or protected airway. A saline cathartic or sorbitol added to the first dose of activated charcoal may speed gastrointestinal passage of the product. In patients who are not fully conscious or have an impaired gag reflex, consideration should be given to administering activated charcoal via a nasogastric tube, once the airway is protected.
Whole bowel irrigation (e.g. 1 or 2 liters of polyethylene glycol solution orally per hour until rectal effluent is clear) may be useful for gut decontamination. Whole bowel irrigation is contraindicated in patients with bowel obstruction, perforation, ileus, hemodynamic instability or compromised, unprotected airways and should be used cautiously in debilitated patients and where the condition may be further compromised. Concurrent administration of activated charcoal and whole bowel irrigation may decrease the effectiveness of the charcoal (there may be competition for the charcoal binding site between the polyethylene glycol and the ingested drugs) but the clinical relevance is uncertain. Prolonged periods of observation (days) may be required for patients who have overdosed with long-acting oxycodone preparations.
If there are signs of clinically significant respiratory or cardiovascular depression, the use of an opioid antagonist should be considered. The opioid antagonist naloxone hydrochloride is a specific antidote for respiratory depression due to overdosage or as a result of unusual sensitivity to opioid. The usual intravenous adult dose of naloxone is 0.4 mg or higher (please refer to naloxone product information for further information). The onset of naloxone effect may be delayed by 30 minutes or more. Concomitant efforts at respiratory resuscitation should be carried out. Since the duration of action of oxycodone, particularly sustained release formulations, may exceed that of the antagonist, the patient should be under continued surveillance and doses of the antagonist should be repeated as needed, or an antagonist infusion established, to maintain adequate respiration.
In an individual physically dependent on, or tolerant to, opioids, the administration of the usual dose of opioid antagonist can precipitate an acute withdrawal syndrome. This may lead to agitation, hypertension, tachycardia and risk of vomiting with possible aspiration. The severity of this syndrome will depend on the degree of physical dependence and the dose of antagonist administered. The use of opioid antagonists in such individuals should be avoided if possible. If an opioid antagonist must be used to treat serious respiratory depression in the physically dependent patient, the antagonist should be administered with extreme care by using dosage titration, commencing with 10 to 20% of the usual recommended initial dose.
Toxicity: Oxycodone toxicity may result from overdosage but because of the great interindividual variation in sensitivity to opioids it is difficult to determine an exact dose of any opioid that is toxic or lethal. Crushing and taking the contents of a modified release dosage form leads to the release of oxycodone in an immediate fashion; this might result in a fatal overdose. The toxic effects and signs of overdosage may be less pronounced than expected, when pain and/or tolerance are manifest.
Hyperalgesia that will not respond to a further dose increase of oxycodone may very rarely occur, in particular at high doses. An oxycodone dose reduction or change in opioid may be required.
As with all opioid preparations, Oxycodone HCl (OxyContin NEO) tablets should be used with caution following abdominal surgery as opioids are known to impair intestinal motility and should not be used until the physician is assured of normal bowel function. Should paralytic ileus be suspected or occur during use, Oxycodone HCl (OxyContin NEO) tablets should be discontinued immediately.
Use caution when prescribing Oxycodone HCl (OxyContin NEO) tablets for patients who have any underlying GI disorders that may predispose them to intestinal obstruction. Patients with underlying GI disorders such as esophageal cancer or colon cancer with a small gastrointestinal lumen are at greater risk.
Oxycodone HCl (OxyContin NEO) tablets should not be taken by patients with difficulty in swallowing or who have been diagnosed with narrowing of the esophagus. If patients experience swallowing difficulties (e.g. choking, gagging, discomfort, regurgitation, tablets stuck in the throat) after taking Oxycodone HCl (OxyContin NEO) tablets, they should be advised to seek immediate medical attention.
Use in chronic, non-malignant pain: The use of Oxycodone HCl (OxyContin NEO) tablets for the treatment of chronic pain which is not due to malignancy should be restricted to situations where: all other conservative non-pharmacological and pharmacological methods of analgesia have been tried and have failed or are insufficient; the pain is having a significant impact on the patient’s quality of life; there is no psychological contraindication, drug-seeking behaviour or past and current personal or family history of alcohol, prescription/illicit drug abuse or misuse.
Opioids, where clinically indicated, should only be prescribed as one component of a comprehensive multimodal management approach to chronic, non-malignant pain. Appropriate patient selection is the key to successful treatment of moderate to severe chronic pain with opioid analgesics.
An initial comprehensive assessment should be conducted using a biopsychosocial approach to identify a cause for the pain and the appropriateness of opioid therapy and to identify psychosocial factors that may exacerbate pain or magnify overall distress (e.g. depression, anxiety, post-traumatic stress disorder, borderline personality disorder, marked family stressors, history of sexual abuse). In the absence of a clear indication for a strong opioid analgesic, drug-seeking behaviour must be suspected and resisted, particularly in individuals with a history of, or propensity for, drug abuse. Factors that may put the patient at increased risk of opioid abuse/addiction include a personal/family history of substance, prescription medication and alcohol abuse, and major psychosocial issues (e.g. psychological/psychiatric disorder). The use of opioids to treat predominant emotional distress should be avoided.
Generally, opioid analgesics are not initiated prior to a full initial clinical assessment and before consideration of other treatment options such as physiotherapy/exercise/rehabilitation approaches, psychosocial interventions such as CBT (cognitive-behavioural therapy) self-management approaches, involvement of a psychologist or psychiatrist to address psychological co-morbidities which may be impacting on pain coping and trials of other non- opioid pharmacotherapeutic or interventional strategies.
Prior to longer-term prescribing, a trial of Oxycodone HCl (OxyContin NEO) tablets or shorter-acting opioid should be undertaken. Longer-term administration of Oxycodone HCl (OxyContin NEO) tablets should only occur if this trial demonstrates that the pain is opioid sensitive. Opioid-naïve patients who require rapid dose escalation with no concomitant pain relief within the trial period should generally be considered inappropriate for longer-term therapy.
One doctor only should be responsible for the prescription and monitoring of the patient’s opioid use. Prescribers should consult appropriate clinical guidelines on the use of opioid analgesics in such patients.
Drug dependence: As with other opioids, tolerance and physical dependence tend to develop upon repeated administration of oxycodone. There is potential for abuse of the drug and for development of strong psychological dependence. Oxycodone HCl (OxyContin NEO) tablets should therefore be prescribed and handled with a high degree of caution appropriate to the use of a drug with strong abuse potential.
Withdrawal symptoms may occur following abrupt discontinuation of oxycodone therapy or upon administration of an opioid antagonist. Therefore, patients on prolonged therapy should be withdrawn gradually from the drug if it is no longer required for pain control.
Oxycodone should be used with caution and under close supervision in patients with pain not due to malignancy who have a prior history of substance abuse. In such cases, prior psychological assessment is essential and the prescribing doctor should consider whether the benefit of treatment outweighs the risk of abuse.
Drug abuse studies: Intranasal abuse: In a human abuse liability study, milled Oxycodone HCl (OxyContin NEO) 30 mg tablets produced subjective responses on each of the four established primary measures that were greater than placebo but significantly less than the responses for another, conventional finely crushed controlled release oxycodone tablets formulation 30 mg, or a fine powder of oxycodone 30 mg when administered intranasally in healthy recreational opioid users with a history of intranasal drug abuse/misuse (n=27). The primary measures were: ‘Drug-liking ‘at this moment”; ‘Overall drug liking’; ‘Subjective Drug Value’; ‘Addiction Research Centre Inventory (ARCI) Morphine Benzedrine Group (MBG)’ scales.
Objective measures of pupil diameter and other subjective measures were consistent with a lower opioid effect. Measurements of intranasal irritation showed increased irritation, particularly related to nasal stuffiness, with Oxycodone HCl (OxyContin NEO) tablets compared with another conventional controlled release oxycodone tablets formulation or oxycodone powder.
In a tolerability and safety study with healthy subjects under fasting conditions, milled Oxycodone HCl (OxyContin NEO) tablets were shown to cause increased nasal discomfort, particularly related to increased nasal stuffiness, and a decrease in runny nose scores when compared with another finely milled controlled release oxycodone tablets formulation, when administered intranasally. Although total AUC was similar for all treatments, Cmax was 67% for coarsely and 77.6% for finely milled Oxycodone HCl (OxyContin NEO) tablets (Ratio of metric means expressed as a percent, transformed back to the linear scale) compared with the other finely milled conventional controlled release oxycodone tablets formulation and Tmax was later with Oxycodone HCl (OxyContin NEO) tablets.
An additional study was conducted to assess the administration site safety and tolerability of intranasally administered milled Oxycodone HCl (OxyContin NEO) tablets placebo vs another crushed conventional controlled release oxycodone tablets formulation placebo. Endoscopy photographs showed residual particles in the nasal cavity at 30 minutes following administration of Oxycodone HCl (OxyContin NEO) tablets placebo.
Accidental or Intentional Oral Misuse: A study in healthy subjects was conducted to characterize the impact of chewing intact and tampered tablets and subsequent swallowing, on the pharmacokinetics of Oxycodone HCl (OxyContin NEO) tablets under fasting conditions. The manufacturing process for Oxycodone HCl (OxyContin NEO) tablets imparts increased hardness to the tablets. Subjects were required to complete a chewing qualification assessment prior to receiving their initial study doses.
The results showed that under both normal and vigorous chewing conditions, Oxycodone HCl (OxyContin NEO) tablets retained some of their controlled release characteristics. Peak plasma levels of oxycodone (Cmax) for Oxycodone HCl (OxyContin NEO) tablets were 13.5% lower when swallowed after vigorous chewing and 23.6% lower when swallowed after normal chewing (Ratio of metric means expressed as a percent, transformed back to the linear scale) when compared with another chewed conventional formulation of controlled release oxycodone tablets. The time to reach peak plasma levels (Tmax) was also delayed for Oxycodone HCl (OxyContin NEO) tablets compared with the other conventional controlled release oxycodone tablet formulation, under both vigorous (1.5 vs 1.0 hours respectively) and normal (2.38 vs 1.13 hours respectively) chewing conditions.
Formulation: Each controlled-release tablet contains: Oxycodone hydrochloride, USP 10 mg, 20 mg, 40 mg.
Oxycodone HCl (OxyContin NEO) tablets are intended for oral use only. The modified release tablets must be swallowed whole, and not broken, chewed or crushed. The administration of broken, chewed or crushed modified release oxycodone tablets leads to a rapid release and absorption of a potentially fatal dose of oxycodone. Parenteral venous injection of the tablet constituents can be expected to result in local tissue necrosis, pulmonary granulomas and serious adverse reactions which may be fatal.
Effects on fertility: In reproductive toxicology studies, no evidence of impaired fertility was seen in male or female rats at oral oxycodone doses of 8 mg/kg/day, with estimated exposure (plasma AUC) equivalent to 8 mg/day in men and 17 mg/day in women.
Despite these fertility studies in animals, prolonged use of opioids may result in impairment of reproductive function, including fertility and sexual dysfunction in both sexes, and irregular menses in women.
Use in Pregnancy: Pregnancy Category C: Drugs which, owing to their pharmacological effects, have caused or may be suspected of causing, harmful effects on the human fetus or neonate without causing malformations. These effects may be reversible.
Oxycodone used during pregnancy or labor may cause withdrawal symptoms and/or respiratory depression in the newborn infant.
Oral administration of oxycodone during the period of organogenesis did not elicit teratogenicity or embryofetal toxicity in rats or rabbits at doses up to 8 mg/kg/day in rats (equivalent to 17 mg/day in women, based on estimated plasma AUC values) or 125 mg/kg/day in rabbits.
Oral administration of oxycodone to rats from early gestation to weaning did not affect postnatal development parameters at doses up to 6 mg/kg/day (equivalent to 9 mg/day in women, based on estimated AUC values). In a study designed specifically to investigate the effect of pre-natal oxycodone on the hypothalamic-pituitary-adrenal axis in adolescent rats, intravenous administration of oxycodone 0.8 mg/kg/day (equivalent to 11 mg/day in pregnant women, based on estimated AUC values) had no effect on the corticosterone response, but delayed and enhanced the peak ACTH response to corticotrophin releasing hormone in males, but not females. The clinical significance of this observation is unknown.
There are no adequate and well-controlled studies with oxycodone in pregnant women. Because animal reproduction studies are not always predictive of human responses, oxycodone should not be used during pregnancy unless clearly needed. Prolonged use of oxycodone during pregnancy can result in neonatal opioid withdrawal. Oxycodone is not recommended for use in women during or immediately prior to labor. Infants born to mothers who have received opioids during pregnancy should be monitored for respiratory depression.
Use in Lactation: Oxycodone accumulates in human milk, with a median maternal milk:plasma ratio of 3:1 recorded in one study. Oxycodone (7.5 ng/mL) was detected in the plasma of one of forty-one infants 72 hours after Caesarean section. Opioids may cause respiratory depression in the newborn and withdrawal symptoms can occur in breastfeeding infants when maternal administration of an opioid analgesic is stopped. Oxycodone HCl (OxyContin NEO) tablets should not be used in breastfeeding mothers unless the benefits outweigh the risks. Breastfed infants should be monitored for respiratory depression, sedation, poor attachment and gastrointestinal signs.
Special Risk Groups: Use in renal and hepatic impairment: In renal and hepatic impairment, the administration of Oxycodone HCl (OxyContin NEO) tablets does not result in significant levels of active metabolites. However, the plasma concentration of oxycodone in this patient population may be increased compared with patients having normal renal or hepatic function. Therefore, initiation of dosing in patients with renal impairment (CrCl <60 mL/min) or hepatic impairment should be reduced to ⅓ to ½ of the usual dose with cautious titration.
Use in the elderly: The plasma concentrations of oxycodone are only nominally affected by age, being approximately 15% greater in elderly as compared with young subjects. There were no differences in adverse event reporting between young and elderly subjects.
Use in elderly, debilitated patients: As with other opioid initiation and titration, doses in elderly patients who are debilitated should be reduced to ⅓ to ½ of the usual doses.
Gender: Female subjects have, on average, plasma oxycodone concentrations up to 25% higher than males on a body weight adjusted basis. The reason for this difference is unknown. There were no significant male/female differences detected for efficacy or adverse events in clinical trials.
Genotoxicity: Oxycodone was not genotoxic in bacterial gene mutation assays but was positive in the mouse lymphoma assay. In assays of chromosomal damage, genotoxic effects occurred in the human lymphocyte chromosomal aberration assay in vitro, but not in the in vivo bone marrow micronucleus assay in mice.
Carcinogenicity: Studies of oxycodone in animals to evaluate its carcinogenic potential have not been conducted.
Driving and operating dangerous machinery: Oxycodone may modify patients’ reactions to a varying extent depending on the dosage and individual susceptibility. If their ability is impaired, patients should not drive or operate machinery.
Oxycodone used during pregnancy or labor may cause withdrawal symptoms and/or respiratory depression in the newborn infant. Oral administration of oxycodone during the period of organogenesis did not elicit teratogenicity or embryofetal toxicity in rats or rabbits at doses up to 8 mg/kg/day in rats (equivalent to 17 mg/day in women, based on estimated plasma AUC values) or 125 mg/kg/day in rabbits.
Oral administration of oxycodone to rats from early gestation to weaning did not affect postnatal development parameters at doses up to 6 mg/kg/day (equivalent to 9 mg/day in women, based on estimated AUC values). In a study designed specifically to investigate the effect of pre-natal oxycodone on the hypothalamic-pituitary-adrenal axis in adolescent rats, intravenous administration of oxycodone 0.8 mg/kg/day (equivalent to 11 mg/day in pregnant women, based on estimated AUC values) had no effect on the corticosterone response, but delayed and enhanced the peak ACTH response to corticotrophin releasing hormone in males, but not females. The clinical significance of this observation is unknown.
There are no adequate and well-controlled studies with oxycodone in pregnant women. Because animal reproduction studies are not always predictive of human responses, oxycodone should not be used during pregnancy unless clearly needed. Prolonged use of oxycodone during pregnancy can result in neonatal opioid withdrawal. Oxycodone is not recommended for use in women during or immediately prior to labor. Infants born to mothers who have received opioids during pregnancy should be monitored for respiratory depression.
Use in Lactation: Oxycodone accumulates in human milk, with a median maternal milk:plasma ratio of 3:1 recorded in one study. Oxycodone (7.5 ng/mL) was detected in the plasma of one of forty-one infants 72 hours after Caesarean section. Opioids may cause respiratory depression in the newborn and withdrawal symptoms can occur in breastfeeding infants when maternal administration of an opioid analgesic is stopped. Oxycodone HCl (OxyContin NEO) tablets should not be used in breastfeeding mothers unless the benefits outweigh the risks. Breastfed infants should be monitored for respiratory depression, sedation, poor attachment and gastrointestinal signs.
Adverse drug reactions are typical of full opioid agonists, and tend to reduce with time, with the exception of constipation. Anticipation of adverse drug reactions and appropriate patient management can improve acceptability. (See Table 2).
 Click on icon to see table/diagram/image
Click on icon to see table/diagram/image
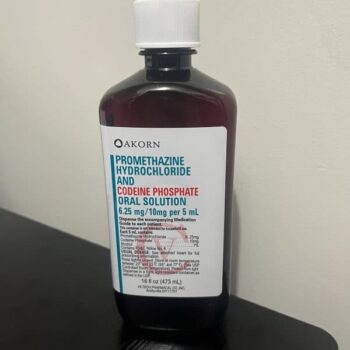
If nausea and vomiting are troublesome, oxycodone may be combined with an antiemetic. Constipation must be treated with appropriate laxatives. Overdose may produce respiratory depression. Compared with other opioids, oxycodone is associated with low histamine release although urticaria and pruritus may occur.
Post-marketing: There have been rare post-marketing cases of intestinal obstruction, and exacerbation of diverticulitis, some of which have required medical intervention to remove the tablet.
There have been uncommon post-marketing reports of difficulty swallowing Oxycodone HCl (OxyContin NEO) 10 mg to 80 mg tablets, potentially due to the swelling and hydrogelling property of the tablets: choking, gagging, regurgitation, tablets stuck in the throat and difficulty swallowing the tablet.
Antihypertensive agents: Hypotensive effects of these medications may be potentiated when used concurrently with oxycodone, leading to increased risk of orthostatic hypotension.
CNS depressants (including sedatives or hypnotics, general anaesthetics, phenothiazines, other tranquillisers, alcohol, other opioids and neuroleptic drugs, etc.): Concurrent use with oxycodone may result in increased respiratory depression, hypotension, profound sedation or coma. Caution is recommended and the dosage of one or both agents should be reduced. Intake of alcoholic beverages while being treated with Oxycodone HCl (OxyContin NEO) tablets should be avoided because this may lead to more frequent undesirable effects such as somnolence and respiratory depression. Oxycodone hydrochloride containing products should be avoided in patients with a history of or present alcohol, drug or medicines abuse.
Coumarin derivatives: Although there is little substantiating evidence, opiate agonists have been reported to potentiate the anticoagulant activity of coumarin derivatives.
CYP2D6 and CYP3A4 inhibitors and inducers: Oxycodone is metabolized in part via the CYP2D6 and CYP3A4 pathways. The activities of these metabolic pathways may be inhibited or induced by various co-administered drugs or dietary elements, which may alter plasma oxycodone concentrations. Oxycodone doses may need to be adjusted accordingly. Drugs that inhibit CYP2D6 activity, such as paroxetine and quinidine, may cause decreased clearance of oxycodone which could lead to an increase in oxycodone plasma concentrations. Concurrent administration of quinidine does not alter the pharmacodynamic effects of oxycodone. CYP3A4 inhibitors such as macrolide antibiotics (e.g. clarithromycin), azole antifungal agents (e.g. ketoconazole), protease inhibitors (e.g. ritonavir) and grapefruit juice may cause decreased clearance of oxycodone which could lead to an increase in oxycodone plasma concentrations. Oxycodone metabolism may be blocked by a variety of drugs (e.g. cimetidine, certain cardiovascular drugs and antidepressants), although such blockade has not yet been shown to be of clinical significance with Oxycodone HCl (OxyContin NEO) tablets.
CYP3A4 inducers, such as rifampin, carbamazepine, phenytoin and St. John’s wort, may induce the metabolism of oxycodone and cause increased clearance of the drug, resulting in a decrease in oxycodone plasma concentrations.
Oxycodone did not inhibit the activity of P450 isozymes 2D6, 3A4, 1A2, 2A6, 2C19 or 2E1 in human liver microsomes in vitro. Non-clinical data in vitro and in vivo indicate that oxycodone can act as a P-glycoprotein substrate and can induce overexpression of P-glycoprotein in rats.
Metoclopramide: Concurrent use with oxycodone may antagonize the effects of metoclopramide on gastrointestinal motility.
Monoamine Oxidase Inhibitors (MAOIs): Non-selective MAOIs intensify the effects of opioid drugs which can cause anxiety, confusion and significant respiratory depression. Severe and sometimes fatal reactions have occurred in patients concurrently administered MAOIs and pethidine. Oxycodone should not be given to patients taking non-selective MAOIs or within 14 days of stopping such treatment. As it is unknown whether there is an interaction between selective MAOIs (e.g. selegiline) and oxycodone, caution is advised with this drug combination.
Neuromuscular blocking agents: Oxycodone may enhance the effects of neuromuscular blocking agents resulting in increased respiratory depression.
Opioid agonist analgesics (including morphine, pethidine): Additive CNS depressant, respiratory depressant and hypotensive effects may occur if two or more opioid agonist analgesics are used concurrently.
Opioid agonist-antagonist analgesics (including pentazocine, butorphanol, buprenorphine): Mixed agonist/antagonist analgesics may reduce the analgesic effect of oxycodone and/or may precipitate withdrawal symptoms.
Shelf-Life: 24 months.

















There are no reviews yet.